Low-Dose CT Screening for Patients at High Risk for Lung Cancer
The United States Preventative Services Task Force (USPSTF) has issued a Grade B recommendation for low- dose CT screening for lung cancer in certain high-risk individuals who:
- Are asymptomatic
- Are between the ages of 55 and 80 years
- Have a history of at least 30 “pack-years” of smoking
- Are either current smokers or have quit in the past 15 years
- Do not have co-morbidities that would prevent effective treatment for lung cancer
Annual screening reduces mortality by 20% in this high-risk population
Screening is not an alternative to quitting smoking
Screening results are presented in a structured reporting system called Lung-RADS
Eligibility Criteria
- Asymptomatic adults
- History of ≥30 “pack years” of smoking
- Current smokers or those that have quit within past 15 years
- Age 55 80 years
- Ability and willingness to undergo curative treatment
The American College of Radiology (ACR) has issued guidelines for the performance of lung cancer screening procedures and standardized reporting using a Lung-RADS lexicon similar to BI-RADS for breast cancer screening.
The aim of this newsletter is to provide information regarding the USPSTF eligibility criteria, the reporting algorithm and recommended management for each category of screening results.
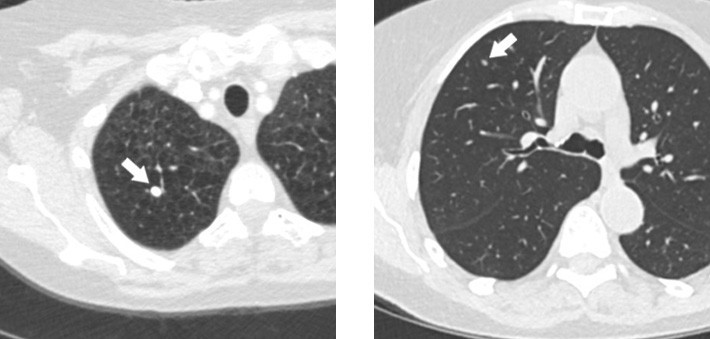
Figure 1. A 69-year-old heavy smoker evaluated with screening CT. An 8 mm calcified nodule in the right lung (arrow) is consistent with a granuloma: LungRADS 1. This is a benign finding and a negative screen. The patient is recommended to return for annual screening 12 months.
Figure 2. A 63-year-old man evaluated with screening CT. Initial screening demonstrates a 5 mm nodule (arrow) that is likely a benign finding: LungRADS 2. The patient was advised to return for annual screening in 12 months.
Smoking Cessation
Screening for lung cancer does not substitute for smoking cessation. All patients undergoing or considering screening should be offered counseling or pharmacotherapy for smoking cessation, which is the most effective way to reduce the risk of lung cancer. Individuals who chose to be screened are likely aware of their risk from smoking and may show increased motivation to quit. Moreover, efforts to help individuals quit smoking increase the cost-effectiveness of screening for lung cancer.
Screening Protocol
The protocol used for lung cancer screening is a low-dose multi-detector helical non-contrast CT scan, which is performed during a single breath hold. Screening scans are repeated annually until an abnormality is detected or the patient no longer fits the criteria for screening. All patients with significant positive findings are no longer considered to be in the screening program but receive further diagnostic tests.
Average Radiation Doses at Mass General for Selected Examinations
| Imaging Examination | Radiation Dose |
|---|---|
| Screening mammography (4 views) | 1.2 mSv |
| Low-dose CT for lung cancer screening | 1.5 mSv |
| Average annual background radiation | 3 mSv |
| Conventional chest CT | 4 mSv |
| CT colonography (screening) | 3-5 mSv |
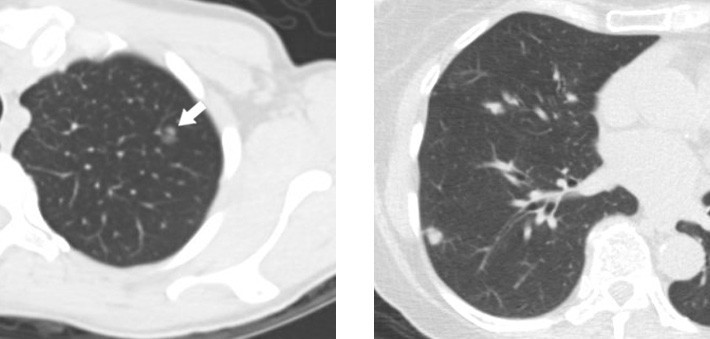
Figure 3. A 70 year old female referred for screening. CT shows a mixed solid and ground glass 7 mm nodule, the solid portion measures 3 mm: LungRADS 3. Follow-up CT recommended in 6 months showed increase in the solid component. Fine needle aspiration showed atypical cells and wedge resection revealed adenocarcinoma.
Figure 4. A 73-year-old woman was evaluated with screening CT. A 10 mm nodule was seen in the lower lobe, consistent with lung RADS 4a. A follow-up low dose-dose CT at 3 months was recommended.
Low-dose CT screening for lung cancer yields a large number of abnormalities suspicious for cancer, most of which are false positives. In the NLST, positive findings (nodules ≥4 mm in any diameter or other abnormalities that were suspicious for lung cancer) were detected in 24.2% of low-dose CT screening studies. Over 95% of these abnormalities were benign on further examination. Subsequent retrospective analysis of the results of another study, the International Early Lung Cancer Action Program, showed that increasing the threshold nodule size to 6 mm reduced the number of positive findings by half without compromising cancer detection. With the higher threshold, only 12% of screening subjects can expect to return for follow-up imaging studies. Approximately 6% will need further evaluation that may require referral to a multidisciplinary clinic comprised of thoracic radiologists, thoracic surgeons, oncologists, and pulmonologists.
The availability of prior chest CT studies at the time of reporting helps the radiologist assess the stability of positive findings and thus reduces the possible need for follow-up.
In the NLST, 4% percent of cancers developed during the interval between annual screenings. These findings indicate that some low-dose CT screening studies are false negatives. Screening may also increase patient anxiety, especially when positive findings appear cancerous.
The radiation dose of a low-dose CT scan is approximately one third that of a standard thoracic CT scan (Table 2). It is comparable to one half of the annual radiation dose due to background radiation at sea level.
The ACR has developed a reporting system for lung cancer screening called Lung-RADS, which is similar in structure to the BI-RADS system for breast cancer screening. It assigns numbers according to the likely severity of the findings and provides recommended actions for follow-up
Summary of the Lung-RADS Reporting System
| Category | Category Descriptor | Primary Category | Management |
|---|---|---|---|
| Incomplete | – | 0 | Additional lung cancer screening CT images and/or comparison to prior chest CT examinations is needed |
| Negative | No nodules and/or definitely benign nodules | 1 | |
| Benign appearance or behavior | Nodules with a very low likelihood of becoming a clinically active cancer due to size or lack of growth | 2 | Continue annual screening with low-dose CT in 12 months |
| Probably benign | Probably benign finding(s) with short-term follow up suggested; includes nodules with a low likelihood of becoming a clinically active cancer | 3 | Low dose CT in 6 months Low-dose CT in 6 months |
| 4A | Low-dose CT in 3 months PET/CT may be used in cases of a ≥ 8 mm solid component | ||
| Suspicious | Findings for which additional diagnostic testing and/or tissue sampling is recommended | 4B | Chest CT with or without contrast PET/CT and/or tissue sampling depending on the probability of malignancy and co-morbidities PET/CT may be used in cases of a ≥ 8 mm solid component |
| *Significant – other | – | S | – |
| *Prior lung cancer | – | C | – |
*Significant – other findings not related to cancer are indicated by the letter S while the letter C denotes prior lung cancer. These letters are used as modifiers to the primary categories 1 4.
When a lung abnormality is observed, a number of characteristics are important for further management including the size of the nodule, whether it is new or existent, whether it is solid or not, and the presence and pattern of calcification. The Lung-RADS system categorizes these findings following precise descriptions to rank cancer risk. The ACR estimates that 90% of screening subjects will fall into Category 1 or 2 and either have no nodules or have those with a very low likelihood of developing cancer (Figures 1 and 2). An estimated 5% of screening subjects will have Category 3 findings that indicate a low (1-2%) likelihood of malignancy (Figure 3). In these cases, a follow-up low-dose CT screening study is recommended after six months. Approximately 4% will be assigned to Category 4, which is divided into two subgroups to account for a higher and lower likelihood of cancer. Patients with findings in Category 4A will be asked to return for a follow-up low-dose CT study in three months or in some cases may be recommended for a PET/CT scan (Figure 4). Those patients who have findings with the highest likelihood of malignancy are assigned to Category 4B. For these patients, follow up depends on the decisions of a collaborative team of radiologists, oncologists, and thoracic surgeons, who may opt for a chest CT with or without contrast, PET/ CT, or biopsy (Figure 5)
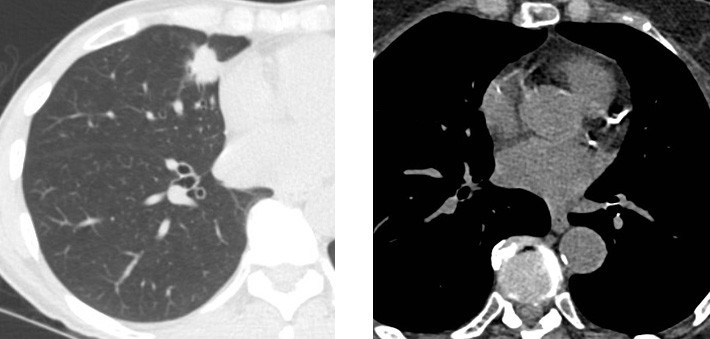
Figure 5. A 58-year-old asymptomatic woman evaluated with screening CT. A 2.2 cm spiculated nodule in the middle lobe is highly suspicious for lung cancer: LungRADS 4b. The patient underwent CT-guided lung biopsy that confirmed adenocarcinoma and the patient was referred for surgical management.
Figure 6. Incidental finding in 73-year-old woman undergoing screening CT. There is heavy coronary artery calcification noted, which is a predictor for cardiovascular disease. No lung nodule was present and the study was categorized as Lung-RADS 1S.
Incidental Findings
In NLST, causes of death other than lung cancer included cardiovascular disease (Figure 6), respiratory disease, and other cancers. While the presence of low-attenuation lesions in the liver, kidneys, and thyroid are of uncertain significance, detection of coronary artery calcification and emphysema can change the management of the patient. Treatment of these diseases can improve outcomes.
Scheduling
Lung cancer screening is offered at the ACE IMAGING, Chembur, Mumbai. Appointments can be made through website (www.aceimaging.in), email (imagingace@gmail.com) or by calling 25288813/8814.
Every effort should be made to obtain prior chest CT studies. The Centre helps in guidance for smoking cessation consultations for patients.
References
Massachussets General Hospital
American College of Radiology (2014) Lung CT Screening Reporting and Data System (Lung-RADS)
http://www.acr.org/Quality-Safety/Resources/LungRADS
Moyer VA (2014). Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 160:330-8
